Chronic Ankle Instability
Chronic ankle instability is one of the most common conditions treated in our clinic.
It is caused by ligament laxity, weakness and a loss of motor control in the affected ankle following a number of recurring sprains over time. Chronic ankle instability can be characterised by either excessive movement of the ankle or by a sense of instability when trying to weight bear through the ankle. Often, patients with the issue will feel as though the ankle is going to “give way” and sometimes the ankle will give way causing a sprain and leading to pain and discomfort.
It can be a very disabling condition for some people, leading to discomfort and fear when walking. This can cause people to avoid doing things they would normally enjoy, such as exercising, as they are in fear of injuring themselves further.
Around 20% of acute ankle injuries may develop into a chronic instability issue. The approach in treating chronic instability differs to that appropriate for an acute ankle injury where tissues need time to settle and heal if possible before targeted therapy is applied.
TREATMENT FOR ANKLE INSTABILITY
Fortunately, chronic ankle instability is a condition that responds well to physiotherapy treatment.
The chronic ankle has failed to gain back its integrity and therefore the approach to treatment can be more focused on strengthening and stability, while also working on any remaining restrictions of movement. Research shows that targeted exercise therapy in particular is highly successful in rehabilitating an unstable ankle.
Your physiotherapist will guide you in the development of a detailed and varied exercise programme. This will typically comprise of balance, strengthening and co-ordination based exercises, specific to you and your ankle. Your physiotherapist will also guide you through the progression of this programme, tailoring it to exactly what activity you are aiming to get back to, and setting specific goals along the way. The aim of physiotherapy in treating chronic ankle instability is to rehabilitate your ankle to a level where you feel ready and confident to take on those activities you enjoy independently.
The Achilles tendon is a tough band of fibrous tissue that attaches the calf muscles to the heel bone. When the calf muscles contract, the Achilles tendon pulls on the heel. This movement allows us to stand on our toes when walking, running or jumping. The Achilles tendon is the largest and strongest tendon in the body, but despite its strength, it is vulnerable to injury. This is due to the high forces placed on it and its limited blood supply.
Achilles tendon pain, often referred to as Achilles tendinopathy, is a troublesome condition, most often seen amongst middle aged to older individuals. This can affect both active and non-active people and is more common in men than women. Although middle age athletes are at a higher risk of developing Achilles tendinopathy, younger athletes can also be affected. Sports and activities that are higher impact and require large forces to be transferred through the Achilles tendon, such as running, jumping, hopping and landing, are more often associated with Achilles tendinopathy.
Achilles tendinopathy is characterised by localised tendon pain particularly when loading the tendon. Injury to the Achilles tendon causes dysfunction and can severely impact recreational and everyday activities.
ACHILLES TENDON PAIN TREATMENT
Many different conservative treatments have been proposed to treat Achilles tendinopathy over the years, including rest, nonsteroidal anti-inflammatory drugs (NSAIDs), ice, massage, electrotherapy and shock-wave therapy. However, research evidence suggests that the best form of conservative management for Achilles tendinopathy is a tailored, patient specific, graded strengthening programme.
Several different strengthening programmes have been studied, each with varying positive effects on Achilles tendinopathy. Some of the strengthening exercises studied include isometric loading (exercise involving a sustained muscle contraction without movement during the contraction), eccentric loading (loading a muscle whilst it is lengthening) and concentric loading (loading a muscle whilst it contracts and shortens).
The type of strengthening exercises prescribed will depend on the presentation of the patient and the physiotherapist’s clinical reasoning. The physiotherapist may focus on one type of muscle contraction or combine several. The exact effect that strengthening exercises have on the Achilles tendon is unclear but it is suggested that they can stimulate remodelling and tissue repair.
Studies have found that an appropriate strengthening programme is not only safe and easy to do, but after just 3 months, many patients return to normal pre-injury levels of running, strength and pain. An appropriate strengthening programme can also help reduce the need for surgery for Achilles pain.
If you are currently struggling with Achilles pain, get in touch with a Physiotherapist here at Ponsonby Physiotherapy. We can advise you on the appropriate strengthening exercises to help resolve your issue.
The most common concerns we see in tennis involve the wrist, elbow, knees and lower back.
The majority of these tennis injuries are due to over use or over load, and they can be easily improved or avoided with some early intervention. Other typical but less common injuries we see are the result of trauma. For example a knee injury from a fall, or a groin injury from an over step and slide, or rushing the net at top speed with cold muscles. Guidance from your coach or physiotherapist on technique and training patterns can go a long way in keeping you active on the court.
Here’s our list of top tennis tips for this season:
#1 Get loose and limber up
Tennis requires fast bursts of activity followed by periods of standing still. Warming up and staying warm is absolutely key to injury prevention. Many a victim have entered our clinic having raced for a drop shot at the net and pulled their calf muscle in the first 10 minutes of a game. Sound familiar? Warming up correctly should include increasing your heart rate, lifting blood flow to muscles and taking your joints through their full range of movement.
See below for an easy 5-10 minute tennis warm up example.
#2 Keep hydrated and fuelled
Hydration is often overlooked in sport. Poor hydration leads to lack of energy and fatigue and lowers concentration. Aim to drink 500-600 mls before you play a match and aim to drink 100-150 mls at the change of ends between games. Alter this according to weather and sweat levels.
Keep easily digestible high energy snacks in your tennis bag. You should try to eat every hour during play depending on the intensity of your game – bananas, fruit bread and cereal bars are all high in carbohydrate and low in fat.
#3 Footwear matters
Correct foot wear choice will be key to preventing lower limb injuries. Your shoes need to provide effective stability from the ground upward as you set your body to play the ball and take on frequent directional changes. Ask your sport shop to direct you towards the tennis, squash or netball section and consider the surface you commonly play on when taking advice – hard court soles will be different to artificial grass or clay.
Inappropriate footwear, with minimal lateral support or structure, can leave you vulnerable to ankle sprains. In addition the stress of maintaining good foot position and lower limb stability may be transferred to the knees and hips. More importantly it affects how well you play the ball!
#4 Avoid tennis elbow
Tennis elbow presents as pain on the outside of the elbow that typically extends down the forearm, sometimes to the wrist. It is a result of inflammation of the attachment of the tendons at the bone on the elbow. In tennis this can be caused by a loose grip on the racket handle, a grip that is too small, playing with wet heavy balls, or a technique that involves excessive wrist movement.
Taping, massage and specific exercises can all help improve the symptoms of tennis elbow, and assessment of your play technique and strength work can prevent the problem from reoccurring. With any tendon issue the sooner it can be assessed and seen the quicker it will recover. 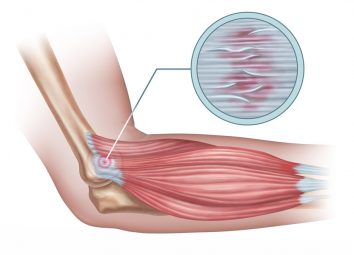
#5 Respond to acute injury
Accidents are sometimes unavoidable, even the best trained players will get injured on court. So what do you do in the heat of the moment and an important match point:
- Establish if you can play on without causing more pain. Take a few minutes to rest, then carefully dummy some shots or go for a short walk or jog at the back of the court. Only play on if you feel confident you can.
- If you choose to discontinue playing adopt the RICED strategy:
-
- Rest: to prevent further damage avoid moving the injured area as much as possible
- Ice: for 20 mins every few hours for the first 48hours
- Compression: Bandage between ice treatments to limit swelling
- Elevate: Keep the injured area above the heart where possible
- Diagnosis: If the pain or swelling hasn’t resolved significantly seek professional help
-
If you are concerned about any pains or niggles this tennis season, book in with one of our physiotherapists here at Ponsonby Physio.
Example of an easy 5-10 minute tennis warm up:
-
- Run 3 laps of the court. At each end change to side stepping along base line facing inward.
- Run at 70% full speed from baseline to net. Jog backwards to the baseline. Repeat 3 times.
- Circle arms 10 times in one direction and 10 times in the opposite.
- Reach hands to the sky then roll down to aim to touch your toes letting your spine roll down from head to toe.
- Lunge walk forwards completing 2 widths of the court.
- Side step into a squat completing 2 widths of the court.
- Where avoidable, never go straight into match play. Hit with a partner in the service boxes for 2-3 minutes before moving to the back of the court to cover the whole court and complete a series of ground strokes, volleys, smashes and serves before you start your game.
Osteoarthritis is the most common arthritis condition which can occur at any age but usually starts after the age of 40. Often previous sporting injuries, and in some cases certain occupations, can place extra load or stress on joints and therefore increase the risk of developing osteoarthritis later in life. For example an ACL rupture of the knee has been shown to increase the likelihood of developing osteoarthritis in this joint at a younger age with increased prevalence.
What is Osteoarthritis?
You may have heard the term wear and tear bandied around in terms of joints, but what does this actually mean to the health of that joint. Cartilage lines the surface of the bones that make up the joint. In a normal healthy joint, the cartilage works as a shock absorber and for providing smooth surfaces between the bones, which allows us to move freely with good movement and no pain.
In the early stage of osteoarthritis, the cartilage starts to thin and then roughens. This process can continue to advance to the point that the breakdown starts to expose the bone and leave it unprotected. This can result in symptoms such as a loss of smooth movement, pain and stiffness.
With the cartilage process breaking down, the bone itself can start to change shape causing the development of bony spurs. These spurs can again further restrict the smooth movement of that joint and cause dysfunction to the soft tissues surrounding the affected joint.
Some of the common areas that are affected by osteoarthritis are the neck and shoulders, lower back, hips, knees and base of toes and thumbs.
What can you do about it?
Although there is no cure for osteoarthritis there are several ways to help control and manage the symptoms of this disease. Nutrition, strength & conditioning exercises and medication will all play a major part. As physiotherapists we are in the ideal position to help you manage your joint symptoms. We can work with you to desensitise structures around the joint with physiotherapy techniques and provide individualised exercises programs that incorporate both strength & conditioning exercises and general aerobic activity.
Exercise has been shown to help with the management of pain and to improve the overall quality of life in those with osteoarthritis. For example, cycling is generally a great way to manage some knee symptoms – it keeps the joint moving and the muscles surrounding the joint strong, as well as providing a level of pain management. Swimming or aquatic exercise offer another low impact cardio based option – beneficial for those suffering from lower back pain associated with osteoarthritis as well as hips, ankles, feet, or shoulder and neck pain.
The design of a resistance conditioning program is a great way to maintain strength around the associated muscle groups, add mobility and function. It will also provide valuable balance input that can help in the prevention of falls or development of other injuries.
Need some help?
If you are unsure of what you could be doing to help manage your osteoarthritis then we would be more than happy to help assist you with this and to help continue with your quality of life. Contact us for an appointment.